Thyroid Cancer Treatment
Once a person is diagnosed with thyroid cancer then they start on the challenging road of finding the most appropriate treatment. That can be hard because there is a lot of information on thyroid cancer treatment, and some choices in terms of how to treat it. In the following I will present the information available to help you decide. The information in this section is limited to treatments for the Differentiated Thyroid Cancers (DTC), including papillary & follicular thyroid carcinomas.
Factors that need to be considered:
- Extent of thyroid surgery
- What to do with the lymph nodes
- Risks associated with different types of thyroid surgeries
- Cure rates
- Recurrence rates
- Cancer follow up
- Radioactive iodine treatment
Thyroid Surgery (Thyroidectomy)
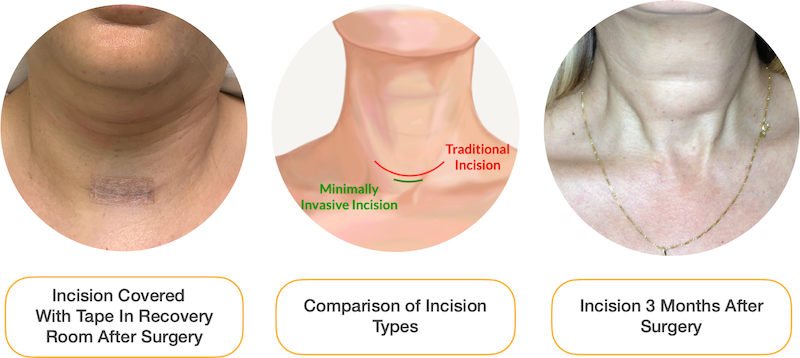
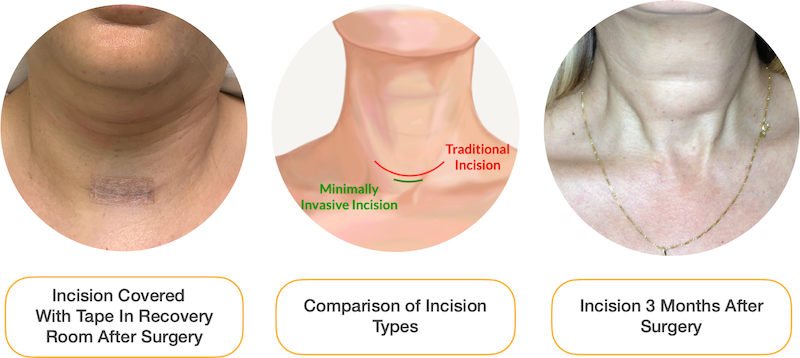
Most Thyroid Surgery Can Be Done Minimally Invasively (Small Incision 3-4cm)
Thyroid surgery is the main treatment for papillary and follicular thyroid cancer. A great majority of the people who have these cancer will have a tumor limited to the thyroid gland and only require surgery and nothing more to be cured. At The CENTER, we will do a full assessment of each patient to see what is the true stage of their tumor, and what are the possible & appropriate surgical options.
There are generally 2 types of thyroid surgeries, and 2 types of surgeries on the lymph nodes when trying to treat thyroid cancer.
- Hemi-Thyroidectomy (or Thyroid Lobectomy)
- Total Thyroidectomy
- Central Neck Dissection
- Lateral Neck Dissection
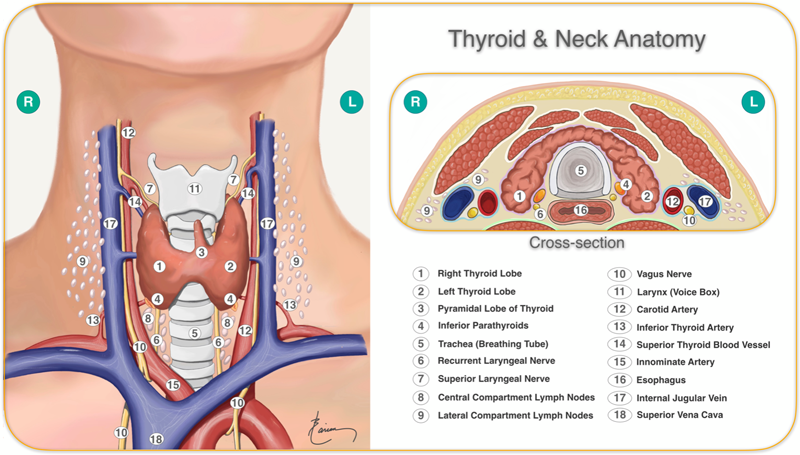
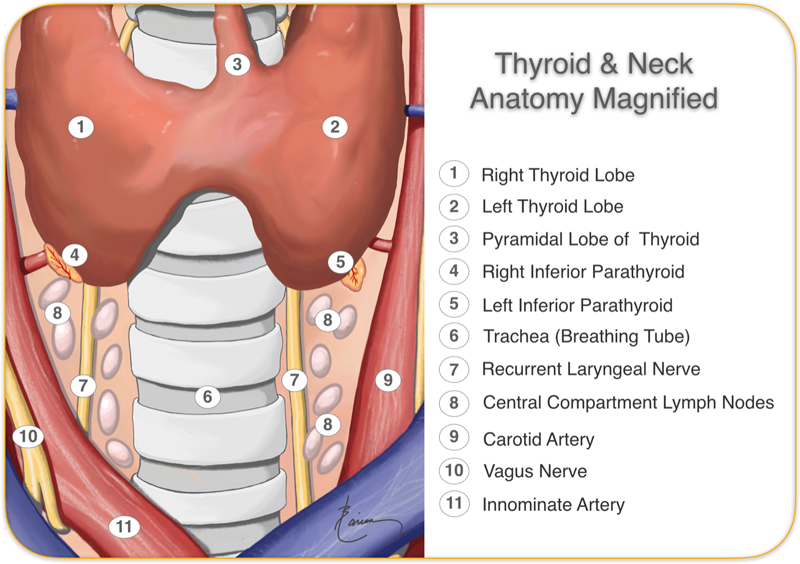
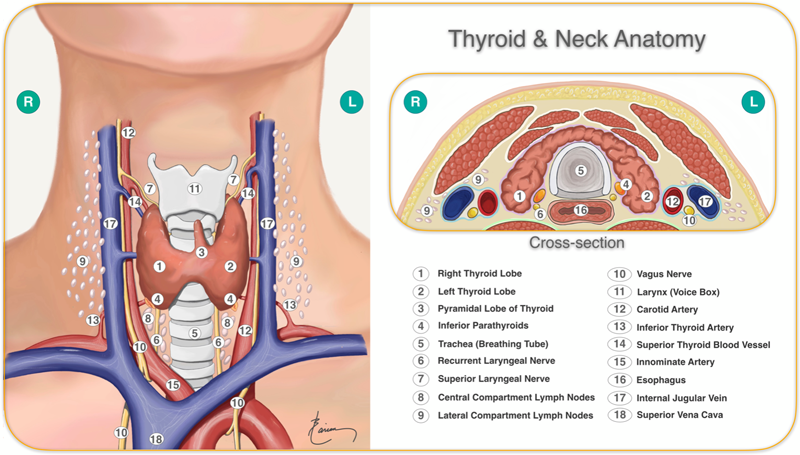
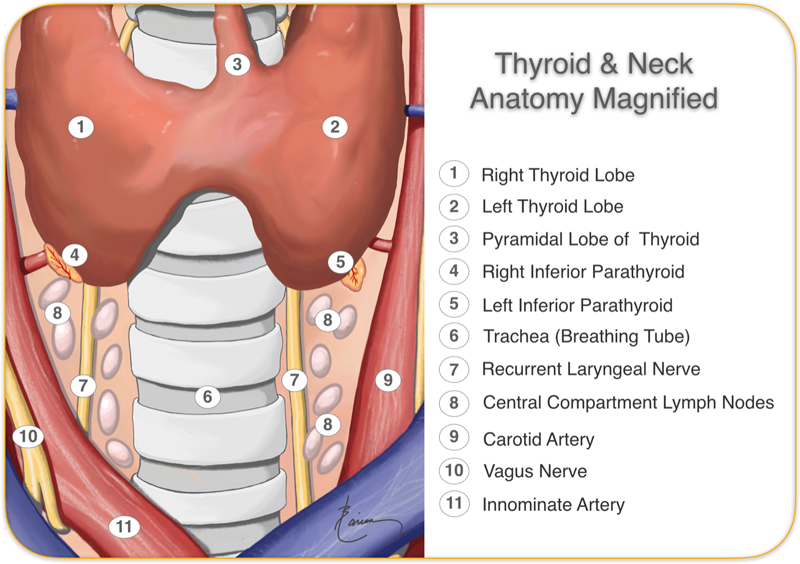
First let’s discuss what each of these surgeries are and then discuss their indication. Below are anatomic diagrams of the neck showing all the relevant structures. In the section following I will show the details of surgeries.
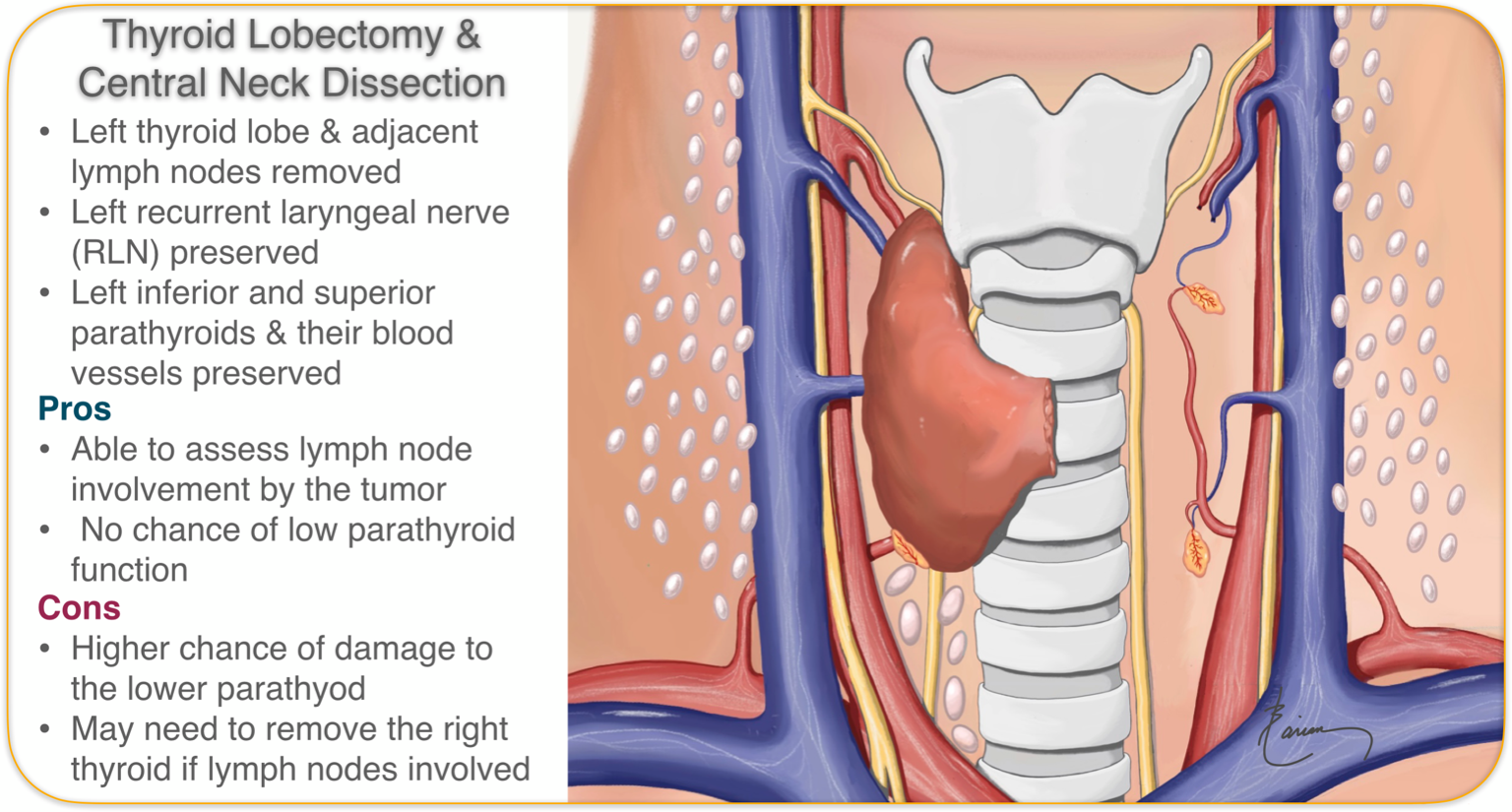
Thyroid Lobectomy
Thyroid lobectomy or hemi-thyroidectomy involves the removal of only half of the thyroid through a very small incision (3 cm, or just over an inch). All of the normal surrounding tissue and organs, including the voice box nerves (recurrent & superior laryngeal nerves), the parathyroids, breathing tube, swallowing tube and blood vessels are seen and carefully preserved so that they function normally. This surgery is done on an outpatient basis and the person may go home and sleep in their own bed the same evening.
The lymph nodes immediately below the thyroid lobe (central compartment lymph nodes) are examined both before the surgery on ultrasound and during surgery by seeing them and feeling them. If on any exam they are suspicious or concerning, then they may be removed as well; this is called central compartment neck dissection. The lymph nodes can then be examined by the pathologist to see if there has been any spread of cancer to them. This will help your surgeon decide if more needs to be done to cure the cancer; such as removing the entire thyroid.
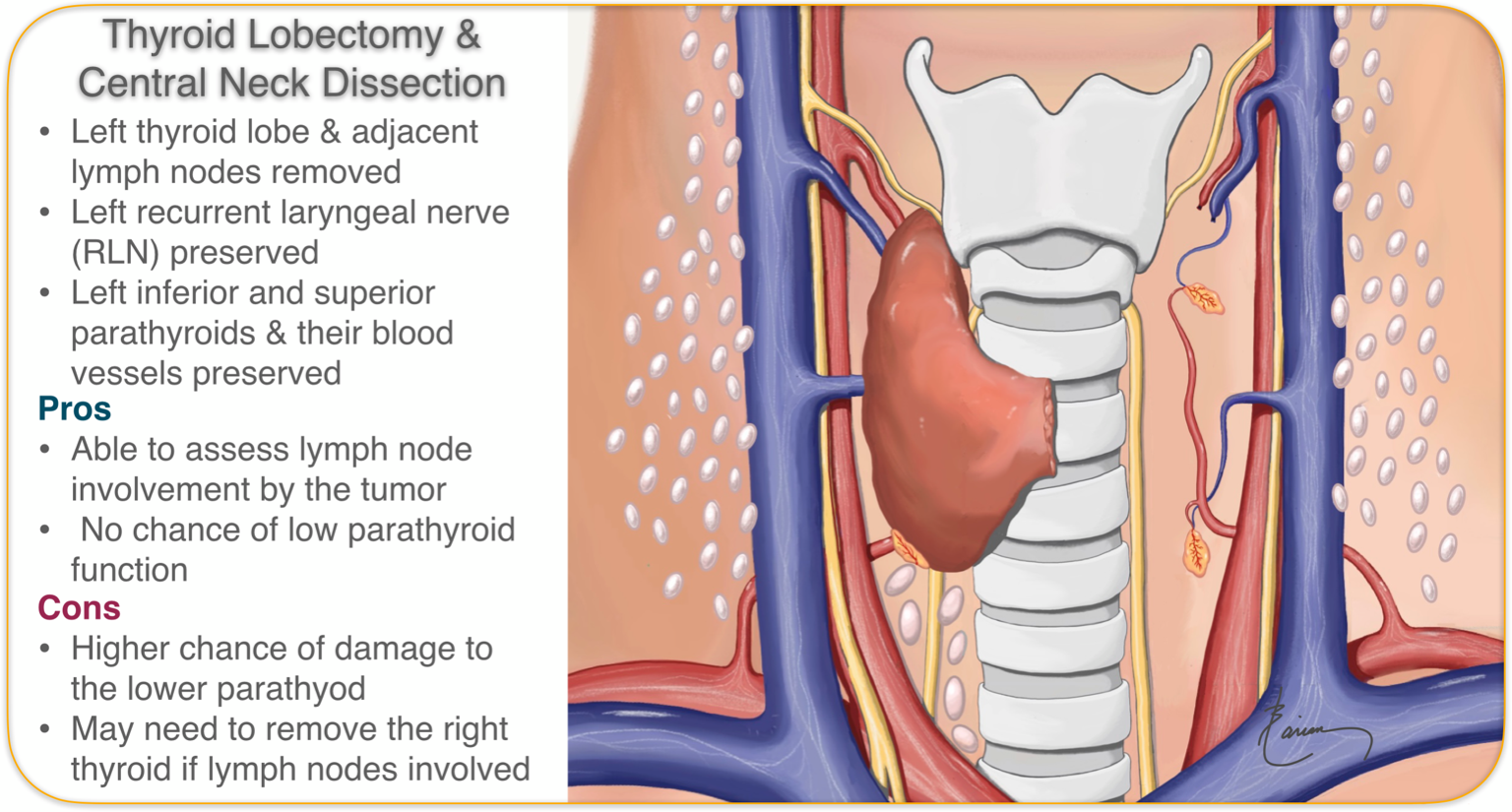
Thyroid Lobectomy Important Facts
- Lobectomy is a very effective treatment for small to intermediate size (less then 4 cm or 1.75 inch) papillary thyroid cancers
- Small well hidden cosmetic incision
- Outpatient surgical procedure
- Essentially no risk of hypoparathyroidism & low blood calcium because only the parathyroid glands on this side are exposed. The parathyroid glands on the opposite side have no risk (we only need one of the four parathyroid glands to work for us to have normal calcium levels)
- Only the voice box nerve on side is visualized during surgery
- Since the other half of thyroid remains and produces thyroid hormones & thryoglobulin
- Majority of people won’t need to take any thyroid hormone pills
- Thyroglobulin levels cannot be used to monitor if the cancer has come back
- Return to essentially normal activities and daily functions within a few days
- No heavy lifting or exercise for three weeks
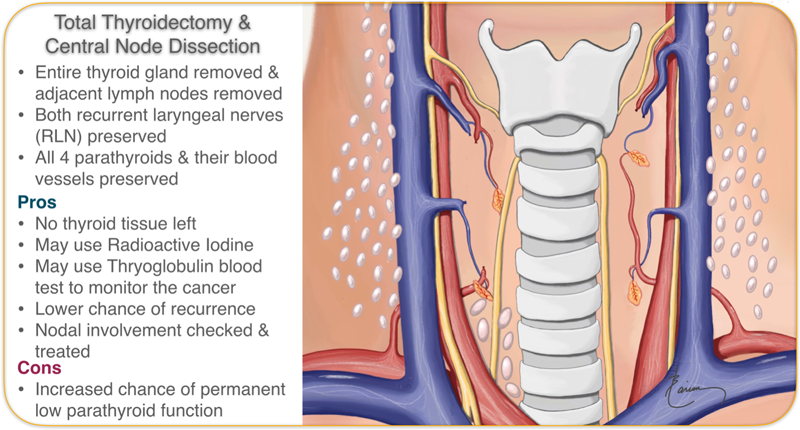
Total Thyroidectomy
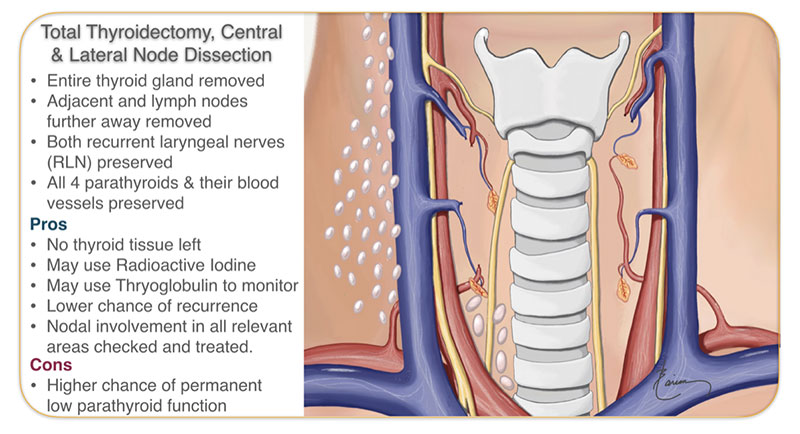
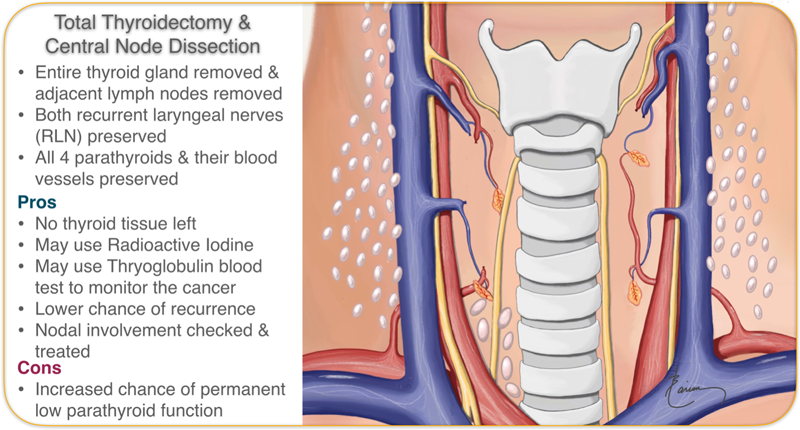
Total thyroidectomy involves the removal of the entire thyroid gland through a very small incision (3 cm, or just over an inch). All of the normal surrounding tissue and organs, including the voice box nerves (recurrent & superior laryngeal nerves), the parathyroids, breathing tube, swallowing tube and blood vessels are seen and carefully preserved so that they function normally. In most instances, this surgery is done with an overnight stay. By the following morning the patient may go home. There is no drain and the incision is closed with absorbable sutures under the skin.

The lymph nodes around the the thyroid (central compartment) and further away to the side (lateral compartment) are evaluated before surgery via ultrasound and during surgery. If any abnormality is seen then the lymph nodes below and next to the thyroid then a central compartment neck dissection is also performed. This means all the lymph nodes next to and below the thyroid is removed going from the breathing tube in the middle to the carotid artery to the side, back to the muscle in front of the spine, all the way down to the upper chest; while the whole time recurrent laryngeal RLN is visualized and protected. All of this is done through the same small incision.
 Before surgery, at the CENTER Dr. Larian performs an ultrasound himself to look at all the lymph nodes; if any of the lateral compartment lymph nodes appear suspicious then he will perform a needle biopsy to see if there is the spread of cancer to the nodes. If that is the case then in addition to a total thyroidectomy, he will recommend doing both a central & lateral node dissection. This does involve making a longer incision to access the nodes to the side.
Before surgery, at the CENTER Dr. Larian performs an ultrasound himself to look at all the lymph nodes; if any of the lateral compartment lymph nodes appear suspicious then he will perform a needle biopsy to see if there is the spread of cancer to the nodes. If that is the case then in addition to a total thyroidectomy, he will recommend doing both a central & lateral node dissection. This does involve making a longer incision to access the nodes to the side.
Thyroid Lobectomy vs. Total Thyroidectomy Recurrence & Cure Rates
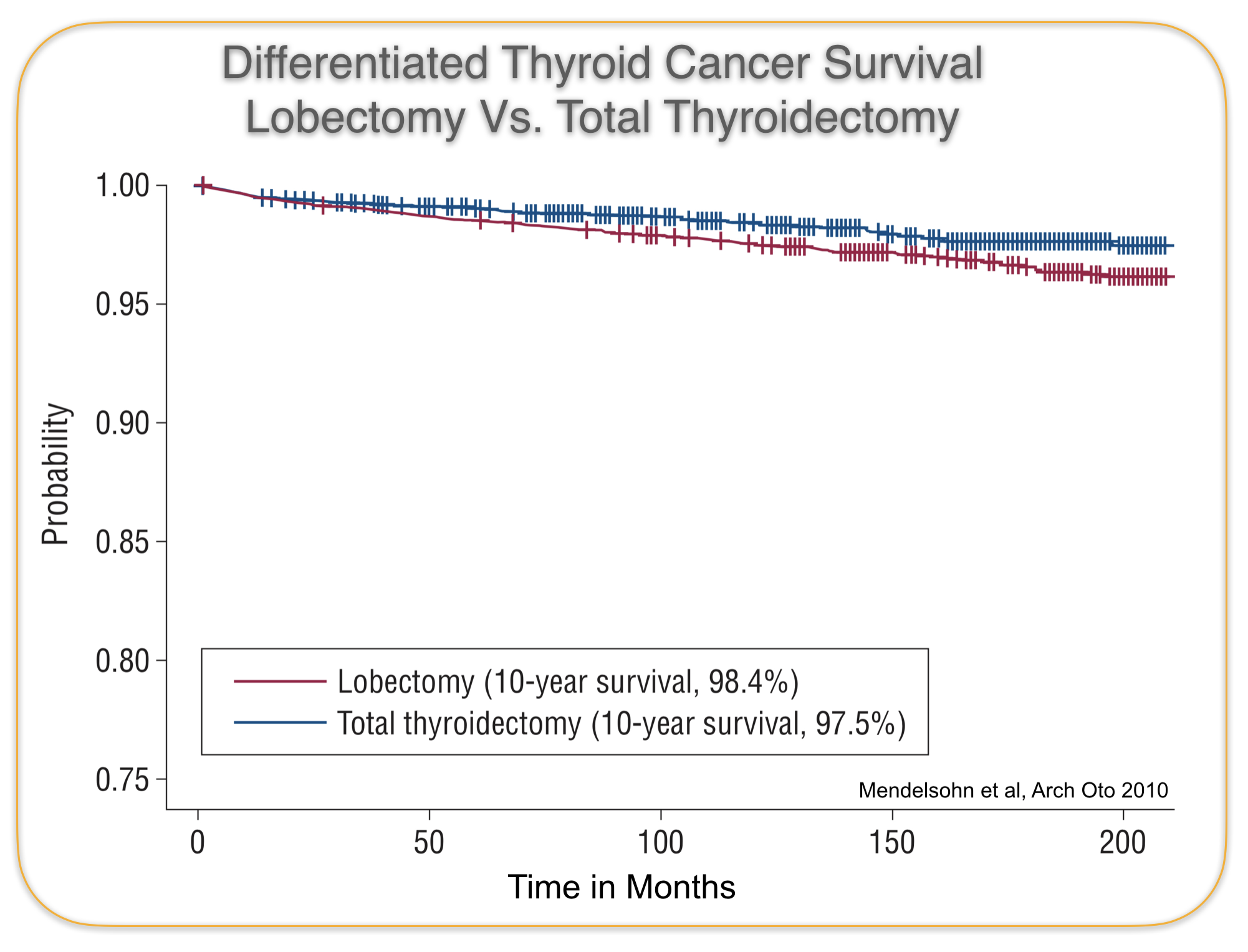
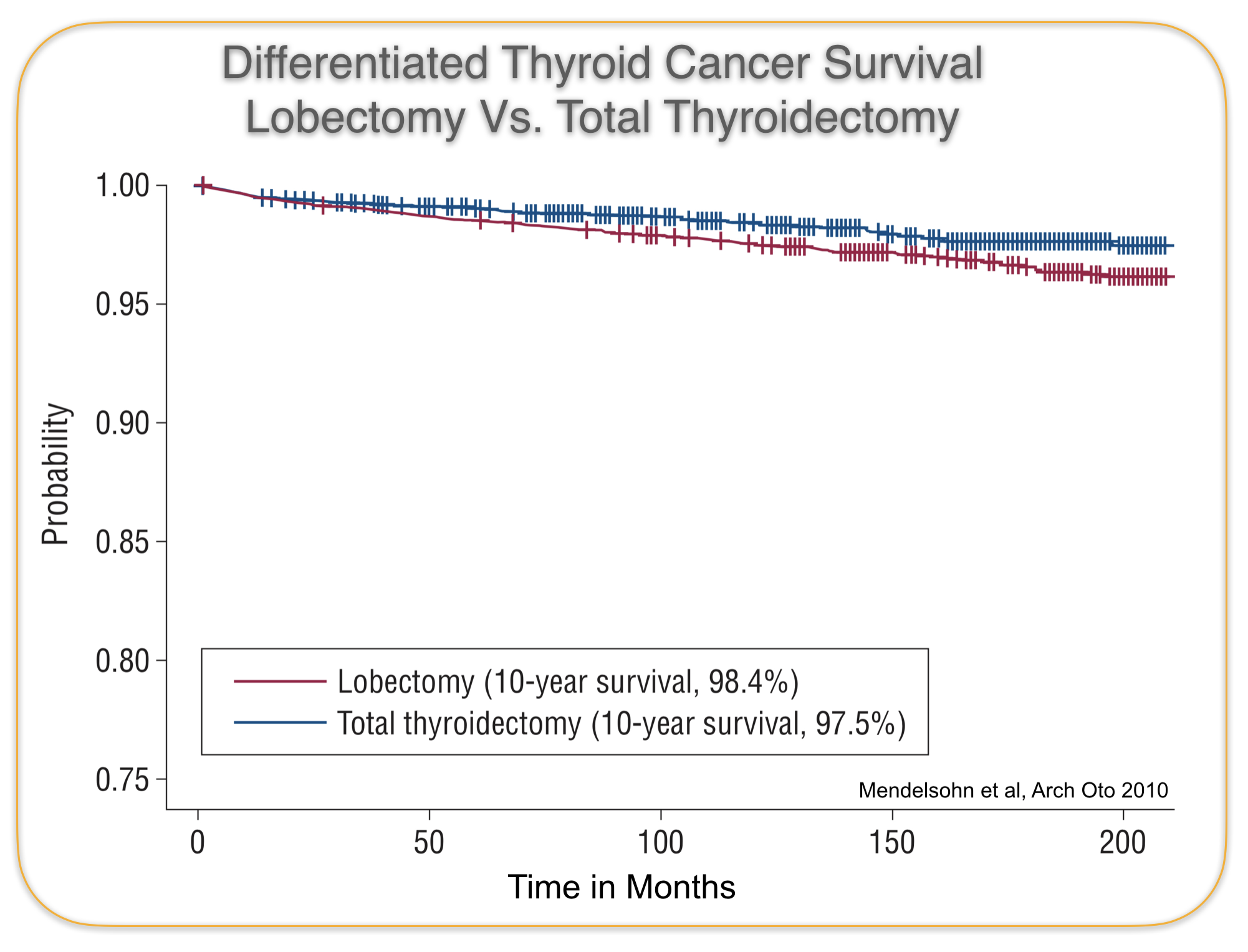
In the past, all people who thyroid cancer were recommended to have a total thyroidectomy. Then researchers looked back at the results and found that 10 year survivals were not significantly different; 97.5% for total thyroidectomy and 98.4% for Lobectomy. There was a small difference in the recurrence rate of thyroid cancer, 9.8% for a lobectomy vs. 7.7% for total thyroidectomy, but that did not seem to impact the ultimate survival rate for the cancer. This means that even though the patients that had a thyroid lobectomy had the tumor come back 2% more then the ones who had a total thyroidectomy, this increased recurrence did not translate into a higher mortality. Or in other words, recurrences can be treated in most cases effectively.
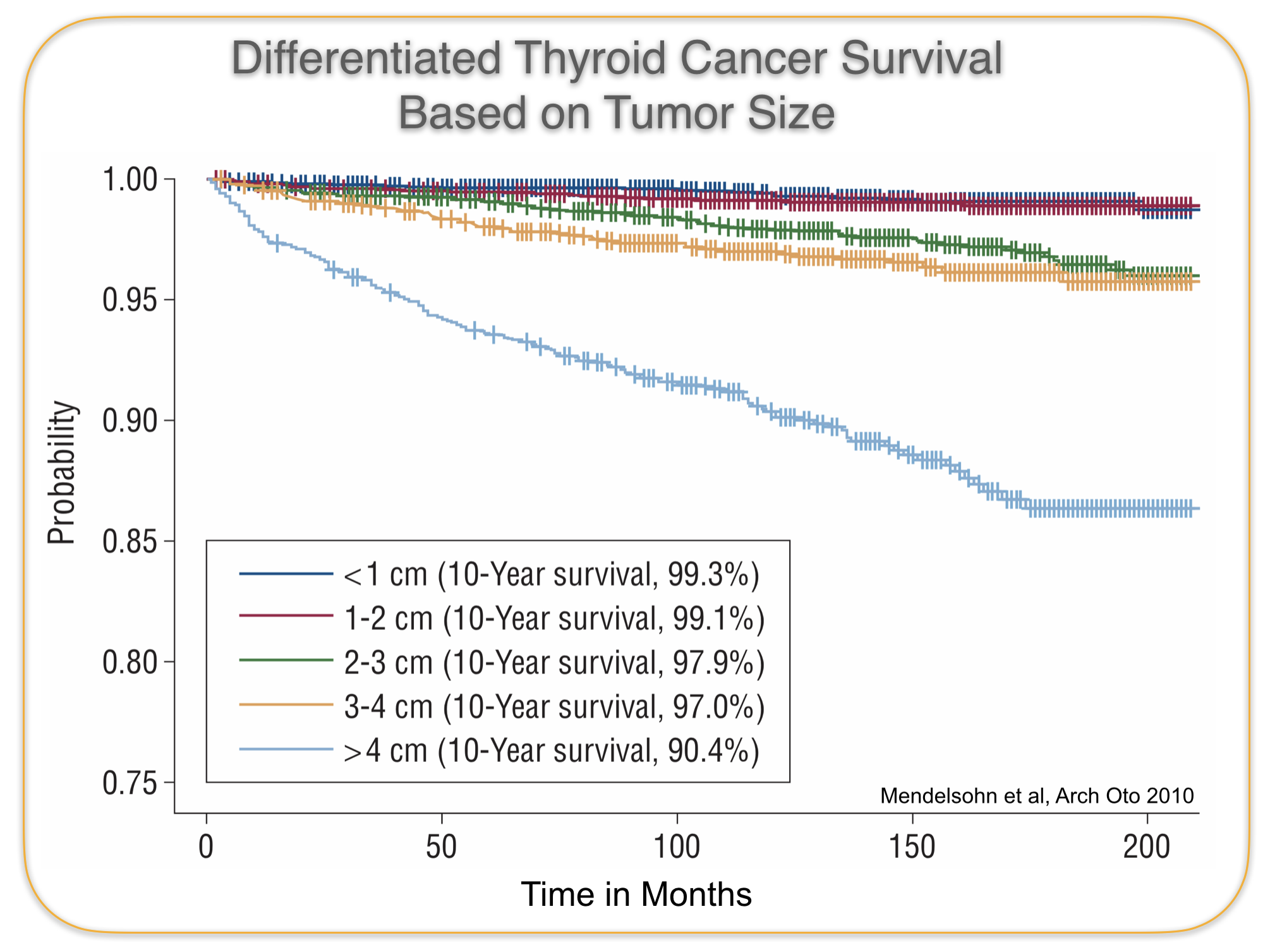
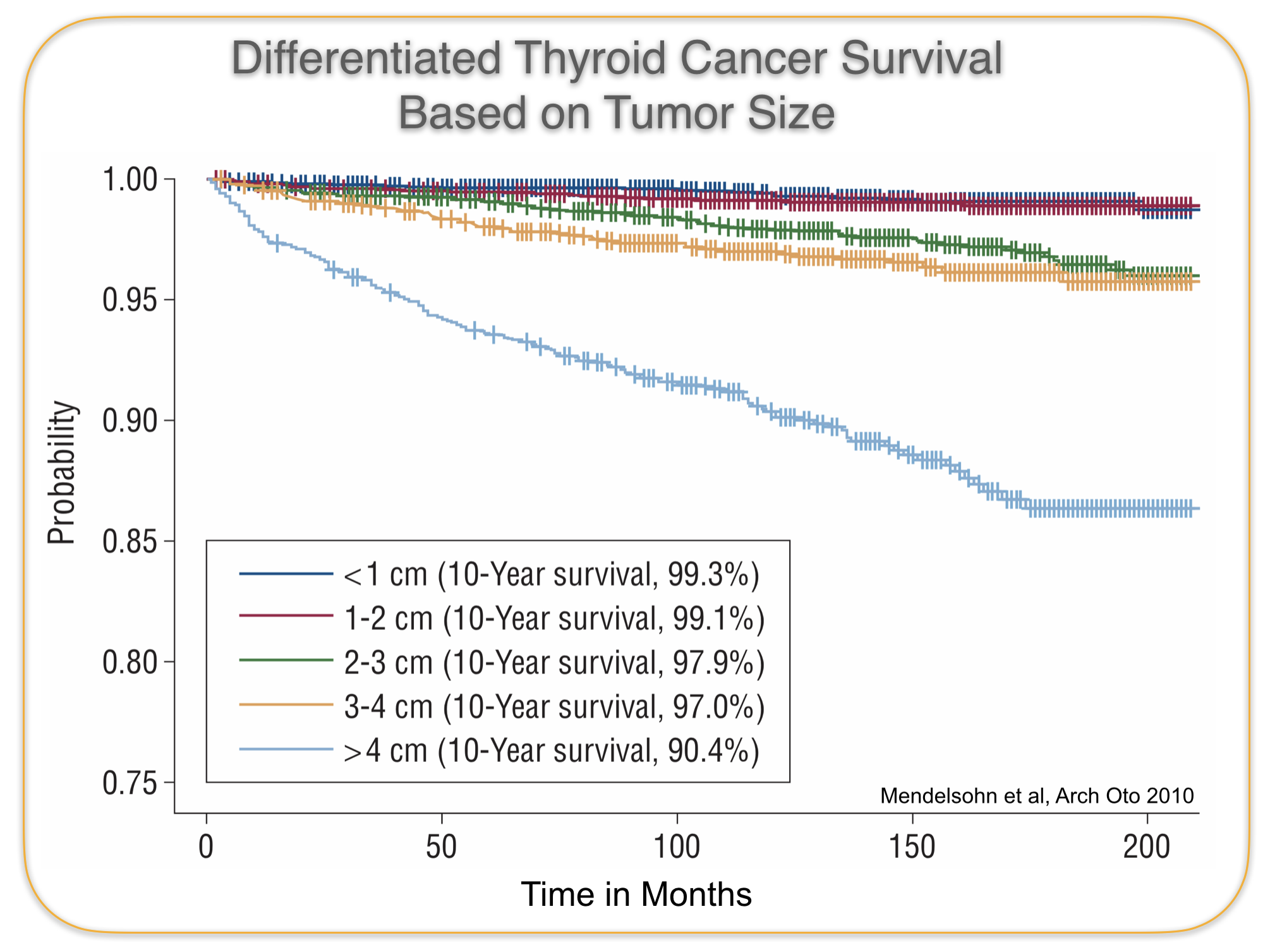
But fortunately there is enough data available to compare size and stage of tumors see the impact on survival for lobectomy vs total thyroidectomy. The data clearly shows that the survival statistics for thyroid cancers that were less then 4cm was significantly better then those that were larger. Therefore all tumors larger then 4cm should be treated with a total thyroidectomy. Other factors that decrease survival probability is extension outside of thyroid, and involvement of multiple lymph nodes. So a lobectomy is most appropriate for a tumor less then 4 cm, that is limited to the thyroid and does not involve lymph nodes.
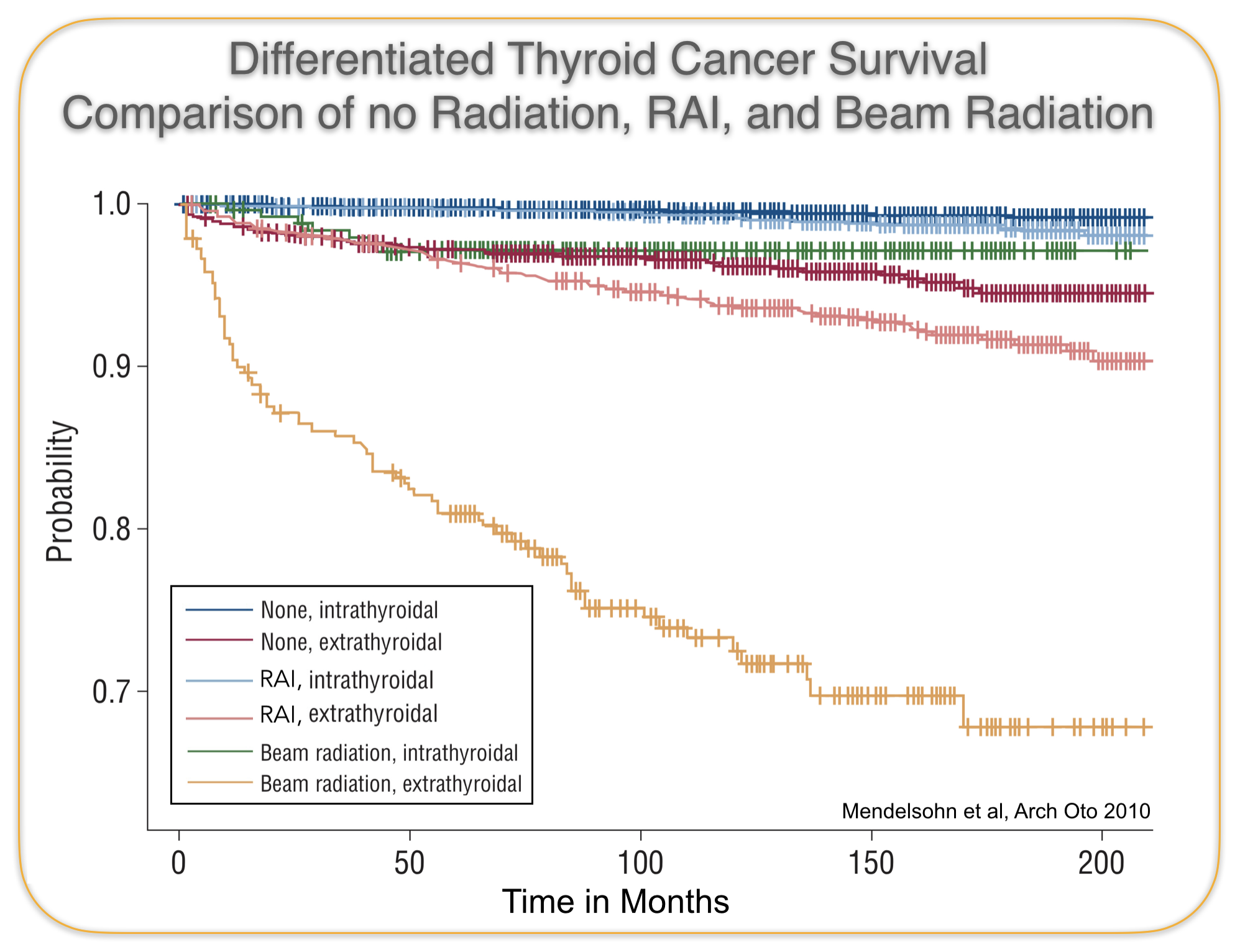
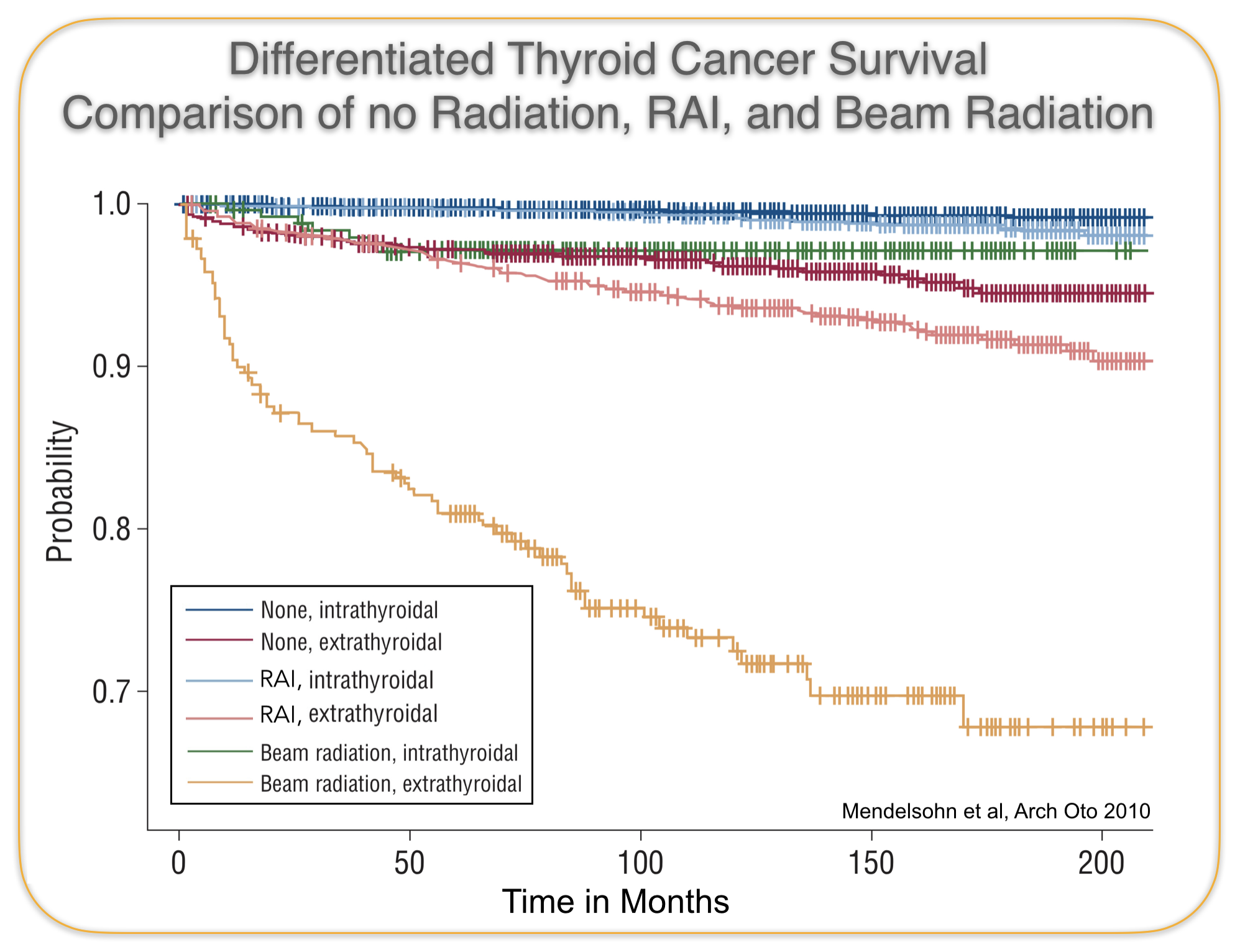
Radioactive Iodine Treatment (RAI)
Iodine is used by normal thyroid cells to make thyroid hormone. On the surface of thyroid cells there is a channel (called the iodine symporter) that allows iodine to get inside. Both papillary and follicular thyroid cancer cells contain this symporter and therefore concentrate iodine inside of them. Once a person undergoes a total thyroidectomy, if a microscopic amount of thyroid cancer cells is still present, getting radioactive iodine would lead to the radioactive iodine concentrating inside the the cancer cells and leading to their demise. This cannot be done if the person still has half of their thyroid because then the radioactive iodine would mostly concentrate in that remaining half of thyroid gland rather then the small amount of cancer cells. So to be able to use RAI a total thyroidectomy must be done. Approximately 15-20% of the thyroid cancers will require RAI treatment, the rest can be cured with surgery alone.




 Before surgery, at the CENTER Dr. Larian performs an ultrasound himself to look at all the lymph nodes; if any of the lateral compartment lymph nodes appear suspicious then he will perform a needle biopsy to see if there is the spread of cancer to the nodes. If that is the case then in addition to a total thyroidectomy, he will recommend doing both a central & lateral node dissection. This does involve making a longer incision to access the nodes to the side.
Before surgery, at the CENTER Dr. Larian performs an ultrasound himself to look at all the lymph nodes; if any of the lateral compartment lymph nodes appear suspicious then he will perform a needle biopsy to see if there is the spread of cancer to the nodes. If that is the case then in addition to a total thyroidectomy, he will recommend doing both a central & lateral node dissection. This does involve making a longer incision to access the nodes to the side.