Thyroid Surgery
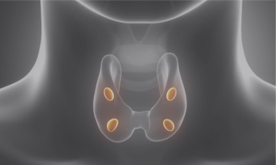
The thyroid is a butterfly-shaped gland that is located in the front lower area of the neck. It is responsible for releasing hormones that regulate growth, metabolism, and heart rate. Problems with the thyroid can trigger unpleasant symptoms and, if untreated, result in serious damage to multiple systems in the body. Likewise, the parathyroid glands, a set of smaller structures located on the back of the thyroid, are essential to normal functioning of the body’s key systems. The job of a parathyroid is to closely regulate the body’s calcium level, keeping the muscles, nerves and other organs working properly. When problems arise, thyroid surgery, performed at our Beverly Hills practice, serving Los Angeles and all of Southern California, may be necessary to restore the body’s natural balance.
Thyroid Problems and Treatments
Problems with the thyroid typically trigger symptoms of either hyperthyroidism or hypothyroidism, as the production of hormones normally secreted by the thyroid is either increased or decreased. Symptoms of hyperthyroidism, or overactive thyroid, include sudden and unexplained weight loss, fatigue, insomnia, shaking, and rapid or irregular heartbeat. Decreased thyroid hormone levels, known as hypothyroidism, can trigger such symptoms as unexplained weight gain, constipation, pain and stiffness in the muscles, and increased sensitivity to cold.
In most cases, these conditions that affect the thyroid hormone production are treated with medications and are best managed by internists and endocrinologists.
 Thyroid Ultrasound
Thyroid Ultrasound
The simplest method to visually examine the thyroid is an ultrasound. Using high-frequency sound waves, we are able to create an image of the thyroid that can reveal any abnormal growth or nodules. Ultrasound cannot be used to determine whether a particular growth is cancerous, however, it can identify the presence, size, and location of the growth, making it possible to access it for a needle biopsy or to use for long-term monitoring of a nodule. There are no risks or side effects associated with ultrasound and it is completely non-invasive. The ultrasound is a very valuable tool in close monitoring after thyroid cancer is removed.dr. larian thyroid surgery
 Fine Needle Aspiration
Fine Needle Aspiration
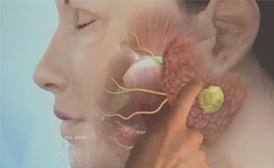
In order to determine whether a thyroid growth is cancerous or not, a sample must be taken and examined for signs of abnormal cells. This can be done by fine needle Fig 4 aspiration, which involves the insertion of a very thin needle through the skin and into the thyroid growth. Ultrasound technology is often used to visualize the internal structures and guide the placement of the needle. Then, cells are collected with the needle so that they can be examined. The physician will generally take multiple samples to ensure an accurate analysis.
Advantages of Minimally Invasive Thyroid Surgery
The incidence of thyroid cancer has been steadily increasing over the past 20 years. Minimally invasive thyroidectomy is a surgical technique to minimize the trauma of surgery and speed up recovery, in addition to using a very small incision. The most important advantage of minimally invasive thyroid surgery (MIT) is a lot less pain after surgery, and therefore minimal use of pain medications. The reason for the less pain is that the technique is, exactly as the title states, less invasive and thus a lot less traumatic to the tissue.
Although the small incision size seems to be a great advantage, and it is, it represents how minimal the trauma to the normal tissue of the neck is in MIT. When the tissue is traumatized less, there is going to be less pain and a lot faster recovery, as well as a much shorter hospital stay.
Our patients who have a total thyroidectomy done, usually stay overnight, and some even go home the same day. Patients who have a hemi-thyroidectomy go home on the same day. The blood loss during MIT is usually minimal and we do not use drains. Due to the ease of the surgery, limited pain and fast recovery, our patients are extremely happy with the results of their minimally invasive thyroid surgery.
Contact Our Practice
To learn more about parathyroid & thyroid surgery, contact our Beverly Hills practice, serving Los Angeles and all of Southern California. Call 310.461.0300!